Introduction
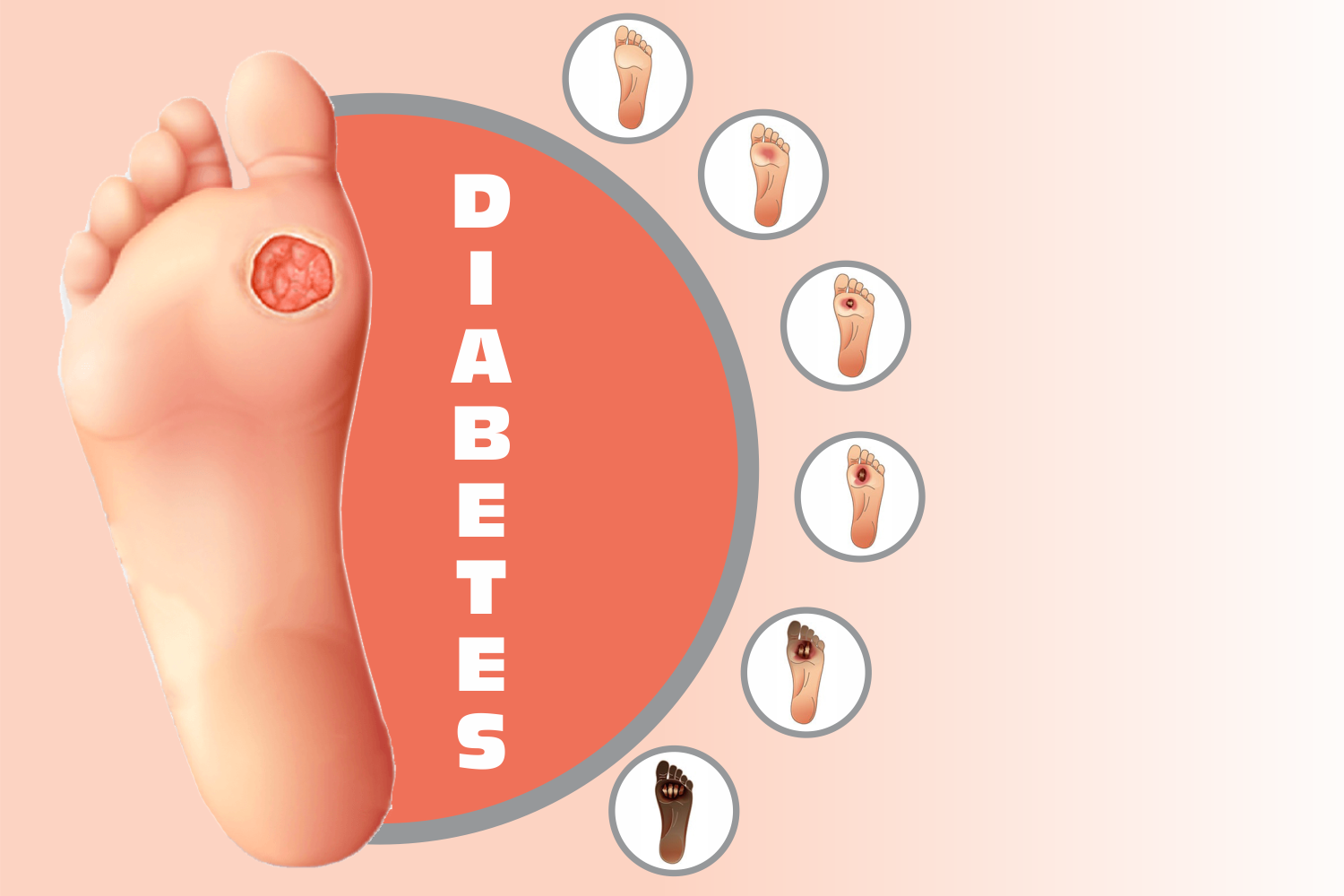
Diabetes allocates a significant proportion of the cost, time, and human resources of the health systems. The rise in industrialization, changes in lifestyle, and food habits have increased the incidence of diabetes and its complications. Diabetes and its complications have become pandemic in the modern era. One such complication of diabetes is Diabetic Foot Syndrome or Disease (DFD). The WHO defines diabetic foot syndrome as an “ulceration of the foot (distally from the ankle and including the ankle) associated with neuropathy and different grades of ischemia and infection.” The critical components of Diabetic Foot Syndrome or Disease (DFD) are diabetic neuropathies and peripheral arterial disease. Chronic hyperglycemia and other risk factors such as tobacco use affect the blood vessels of the feet, and this condition is called Peripheral Arterial Disease (PAD). Diabetic foot syndrome or disease is considered to be a medical condition with an economic burden. It is limb-threatening and sometimes life-threatening, as it may lead to amputation if osteomyelitis is involved.
Symptoms of Diabetic Foot syndrome
Diabetic patients are advised to report their physician immediately if they have any of the following symptoms:
- Change in the color of their skin
- Swelling in the foot and ankle accompanied by severe pain in the legs.
- Ulcers on the feet take a longer time to heal.
- Onychomycosis ( Fungal infections of the toenail)
- The skin layer becomes thick, hardened and the inflammation or small blisters are mainly present on the sides of the feet and between the toes. This is known as corn.
- Foul odor coming from the foot that does not go away
- Loss of hair from feet or legs
- Numbness ( loss of feeling in the feet or legs)
- Colour of the nail turning yellow
Risk Factors for Diabetic Foot Syndrome
The risk factors for Diabetic Foot Syndrome include:
- Chronic Hyperglycemia
- Diabetic Neuropathy
- Peripheral Arterial Disease
- Excessive use of tobacco by diabetes patient
- Diabetic Kidney Disease
- Hypercholesterolemia
- Obesity
- High plantar foot pressures
- History of foot ulcers in diabetic patients.
Complications due to Diabetic Foot Syndrome
Diabetic foot disease is a dangerous disease and needs immediate clinical intervention. Poor diagnosis, lack of proper treatment, and lack of education & management in patients with Diabetic Foot disease can lead to the following complications:
- Infections to the skin and bone due to damage to the nerve and blood vessel.
- Formation of Abscess or pus
- Gangrene
- Muscle deformities due to nerve damage
- Charcot foot; a condition of weak bones and loss of sensation in the foot due to diabetes
- Amputation of limb
How is Diabetic Foot Syndrome diagnosed?
The main objective of diagnosis is to identify the severity of diabetic foot ulcers. This prevents the complications mentioned above and develops specific treatment & prevention measures to combat diabetic foot disease or diabetic foot ulcers (DFU). To make things simple, the International Working Group of the Diabetic Foot (IWGDF) set the Perfusion, Extent, Depth, Infection, and Sensation (PEDIS) classification system in which all DFUs are classified according to four PEDIS grades as mentioned in the table below:
| PEDIS GRADE | INFECTION SEVERITY | CLINICAL MANIFESTATIONS |
|---|---|---|
| 1 | Uninfected | Lack of manifestations of inflammation |
| 2 | Mild | Presence of two or more manifestations of inflammation like purulence, erythema, tenderness, warmth, or induration. The ulcer is limited to the skin with no other complications or illness. |
| 3 | Moderate | The clinical manifestations are similar to grade 2 but with the additional clinical symptoms:
|
| 4 | Severe | Patient is metabolically unstable and has the following clinical conditions:
|
Once the diabetic patient with DFD symptoms visits a physician, the physician tries to identify the severity of the infection, as mentioned in the above table. First, the physician checks the patient history to find if the patient has any other medical condition apart from diabetes like peripheral neuropathy and peripheral arterial disease. Next, the physician directs the patient for a blood glucose test to check the severity of diabetes. Physical examination of the patient’s foot, toes, and toenails to study the occurrence of blisters or corn or calluses and any numbness in the foot is a significant part of diagnosing diabetic foot ulcers or disease. The physician also checks the pulse to evaluate the blood flow rate in the foot, the shape of the foot, and the patient’s walking style.
If the physician doubts the alignment of bones in the foot, the patient may have to go for an X-ray imaging test. An X-ray test assesses the bone mass and changes in the alignment of bones in the foot, thus preventing any new ulcer from developing in the future.
If the physician needs more information on the damage done by the ulcer on the patient’s foot, then the patient may have to undergo an MRI Scan.
Finally, to confirm diabetic foot disease, the physician may carry out a biopsy (take a sample of skin from the foot) and send it to the laboratory for microscopic examination.
Based on the clinical manifestations and laboratory tests, a physician develops confidence about the severity of the disease and proceeds towards treatment and management.
Conclusion
Diabetic Foot Disease puts a tremendous burden on the family, healthcare staff, services, and society. Proper education to diabetic patients and their relatives about the cause, symptoms, complications, diagnosis, prevention, multi-disciplinary treatment, and close monitoring is the need of the hour. Every diabetic patient should carry out an annual medical examination to detect possible risks of foot disease. Rather than simply responding to acute problems as they arise, there should be an overall system in place to satisfy the needs of patients who require chronic care. There should be programs to increase global awareness of diabetic foot disease and stimulate this transformation of international guidelines into local guidelines, leading to improved diabetic foot care management worldwide.
References
- Aalaa. M, et al-(2012) / Nurses’ role in diabetic foot prevention and care; a review / J Diabetes MetabDisord. 2012; 11: 24 / Available at
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3598173/ - Guell C, Unwin N. Barriers to diabetic foot care in a developing country with a high incidence of diabetes related amputations: an exploratory qualitative interview study. BMC Health Serv Res. 2015 Sep 14;15:377. doi: 10.1186/s12913-015-1043-5. PMID: 26369788; PMCID: PMC4570260.
- Monteiro-Soares M, Russell D, Boyko EJ, Jeffcoate W, Mills JL, Morbach S, Game F; International Working Group on the Diabetic Foot (IWGDF). Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3273. doi: 10.1002/dmrr.3273. PMID: 32176445.
- Diabetic Foot Problems. Accessed at https://www.webmd.com/diabetes/foot-problems
- Diagnosing Diabetic Foot Ulcers. Accessed at
https://nyulangone.org/conditions/diabetic-foot-ulcers-in-adults/diagnosis - Diabetic Feet. Accessed at https://my.clevelandclinic.org/health/diseases/21510-diabetic-feet#diagnosis-and-tests