Introduction
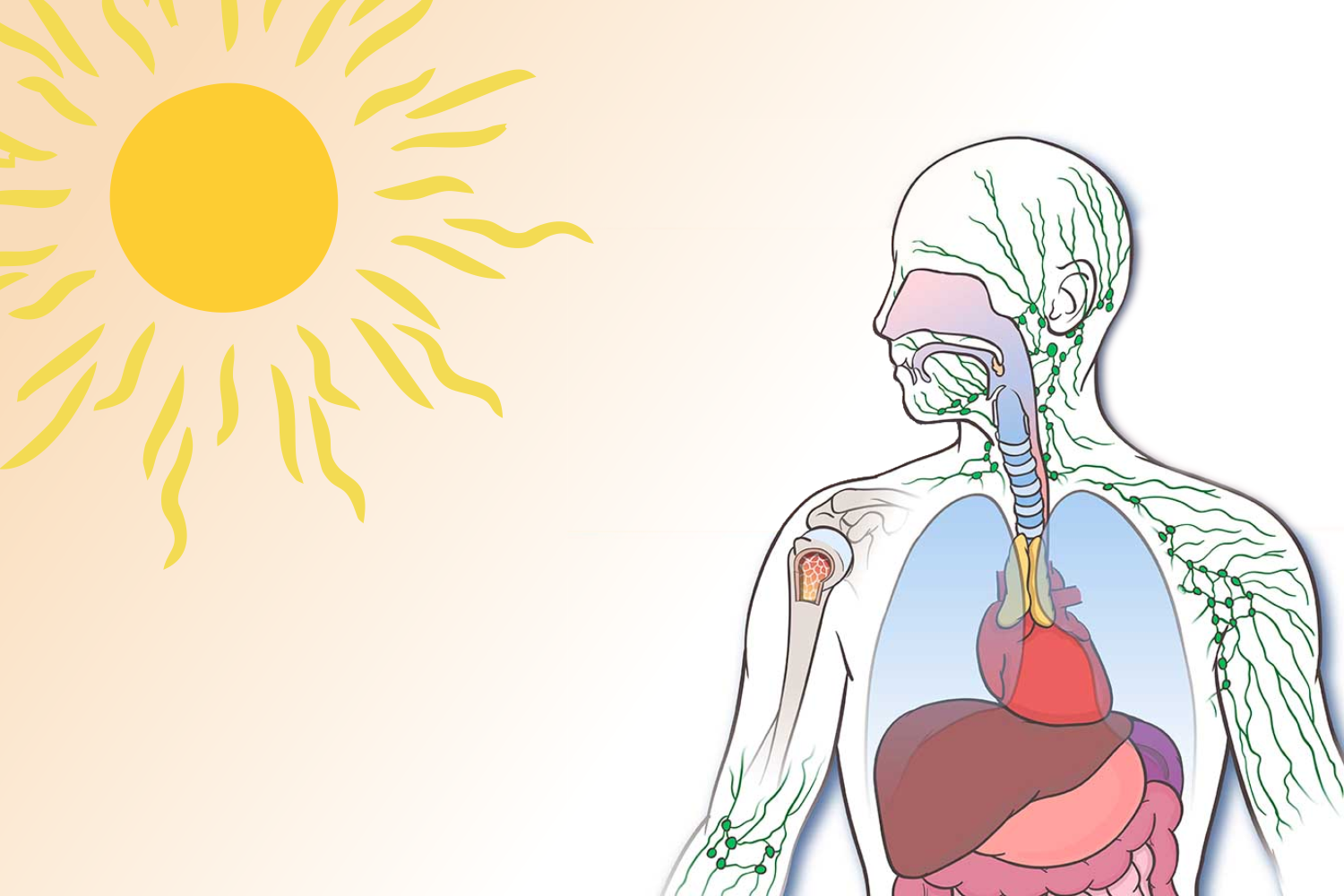
Most people are unaware that Vitamin D, known as the sunshine vitamin, is a hormone. In reality, the result of Vitamin D conversion in the human body is considered a hormone. This is because 90% of Vitamin D in human beings is obtained from sunlight. Food items rich in Vitamin D include fatty fish, egg yolks, fortified milk, oranges, and wild mushrooms. The human skin absorbs the sunlight (especially UV-B radiation), and the synthesis of Vitamin D occurs in the liver and kidneys. Synthesis of Vitamin D continues in the liver and kidneys until the final active form of the hormone is produced.
Vitamin D is necessary for the immune system’s health and function. Vitamin D increases the pathogen-fighting abilities of monocytes and macrophages — white blood cells that play a crucial role in immune protection — and helps relieve inflammation, which aids immunological response. In addition, vitamin D receptors are found in various cells throughout the body, including immune cells, and allow them to respond to Vitamin D molecules, causing multiple physiological effects. So it’s no surprise that Vitamin D has such a wide range of health implications, including bone health, cardiovascular health, immunity, autoimmune illness, type I diabetes, and mental health.
Vitamin D’s ability to regulate immunity through effects on both the adaptive and innate immune systems has gained much attention. This is partly due to research was done more than a century ago by Dr. Nils Finsen, a relatively unknown scientist at the time. Dr. Finsen earned the Nobel Prize in Medicine or Physiology in 1903 for demonstrating that focused light irradiation might treat the epidermal form of tuberculosis (TB), lupus vulgaris. Further research documenting the successful use of oral vitamin D supplementation to treat lupus vulgaris and other mycobacterial illnesses such as leprosy led to the discovery that exposure to ultra-violet light stimulates epidermal vitamin D production.
With the advent of antibiotic therapies, these studies remained confined to history books. However, Finsen’s work was thrust back into the spotlight in 2006 due to a series of genome-wide analyses. The genome-wide analyses revealed pathogen-induction of an intracrine vitamin D system in monocytes, as well as an associated mechanism for vitamin D’s anti-mycobacterial effects, while also shedding light on how these responses may vary depending on an individual’s vitamin D “status.”
There are two types of immunity: innate immunity and adaptive immunity. The natural immune system (responsible for swiftly combating infections) and adaptive immune system (which produces a slower response but is highly specialized, e.g., responsible for producing antibodies) are vital in fighting infections. Both methods appear to be regulated by vitamin D, which explains why this hormone has a broad impact on the immune system. Vitamin D is known to play a function in autoimmune as well. Vitamin D deficiency is common in people with inflammatory diseases like rheumatoid arthritis, lupus erythematosus, and bowel disease.
Vitamin D deficiency is found to be associated with the development of a variety of type one (Th1) mediated autoimmune illnesses, such as type 1 diabetes, multiple sclerosis (MS), and inflammatory bowel diseases (IBD). Furthermore, it has been demonstrated that the active form of vitamin D (1,25(OH)2D3) entirely prevents the development of these autoimmune disorders in experimental models.
Vitamin D deficiency increases the chances of infection.
According to a study, people with low vitamin D levels are more likely to have infections in their upper respiratory tract (URTI) than those with sufficient levels in their bodies. However, a decrease in Vitamin D levels has been linked to an increased risk of illness, particularly influenza. For instance, a study found that daily Vitamin D supplementation for 15 to 17 weeks during the winter reduced the occurrence of influenza infections in Japanese children by 42 percent compared to a control group. Another study found that Vitamin D supplementation for three months during the winter in children with Vitamin D deficiency reduced upper respiratory tract infections.
A new study of 216 persons with COVID-19 discovered that 80 percent of them had insufficient vitamin D levels in their blood. The study also reported that people with both COVID-19 and low vitamin D levels had a higher number of inflammatory markers like ferritin and D-dimer, linked to poor COVID-19 outcomes. Maintaining adequate vitamin D levels, according to medical experts, may help minimize risk or aid recovery from severe COVID-19 in some people. However, scientists believe that further research is needed.
How can Vitamin D levels be improved?
The most natural and preferable approach to receiving enough Vitamin D is regular exposure to sunlight. Aiming for 10-20 minutes of sun exposure several times a week is usually a fair balance between necessary Vitamin D levels and avoiding skin cancer risk. Therefore, we are more likely to meet our daily Vitamin D requirements from sunlight exposure during the spring and summer months.
For around two months, vitamin D is stored in the body. As a result, the Vitamin D you built up during the sunny days will disappear during winter. However, since it’s challenging to acquire enough Vitamin D from diet alone, the best way to meet one’s daily requirements in winter is through supplements.
Vitamin D3 or D2 supplements are the most common, with D3 being more effective at raising Vitamin D levels in the body. In addition, supplements are available in pill form and sublingual drops or spray, ideal for individuals who suffer from malabsorption.
How much Vitamin D should you take?
There are many different expert viewpoints regarding how much Vitamin D we should take as supplements. According to the Department of Health’s recommendations, anyone over four should take ten micrograms (400 IU) of vitamin D daily, especially between October and March. People at increased risk (little or no exposure to sun and people with dark skin complex) should take Vitamin D supplements all year. The Department of Health also recommends a daily limit of 100 micrograms (4000 IU).
However, Vitamin D requirements vary widely depending on where you live (people in northern regions have a high risk of Vitamin D deficiency), age, season, and individual variables (some people may require more Vitamin D than others).
References
- Aranow, C. (2011). Vitamin D and the immune system. J Investig Med., 59(6), 881–886.
- Baeke, F., Takiishi, T., Korf, H., Gysemans, C., & Mathieu, C. (2010). Vitamin D: Modulator of the immune system. Current Opinion in Pharmacology.
- Cantorna MT, Yu S, Bruce D. The paradoxical effects of vitamin D on type 1 mediated immunity. Mol Aspects Med. 2008 Dec;29(6):369-75. DOI: 10.1016/j.mam.2008.04.004. Epub 2008 May 4. PMID: 18561994; PMCID: PMC2633636.
- Chen S, et al. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol. 2007;179(3):1634–47
- Holick, M. F., Binkley, N. C., Bischoff-Ferrari, H. A., Gordon, C. M., Hanley, D. A., Heaney, R. P., et al. (2011). Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 1911–1930. DOI: 10.1210/jc.2011-0385
- Liu, P. T., Schenk, M., Walker, V. P., Dempsey, P. W., Kanchanapoomi, M., Wheelwright, M., et al. (2009). Convergence of IL-1beta and VDR activation pathways in human TLR2/1-induced antimicrobial responses. PLoS ONE 4:e5810. DOI: 10.1371/journal.pone.0005810
- Wang, X., Gocek, E., Liu, C. G., and Studzinski, G. P. (2009). MicroRNAs181 regulate the expression of p27Kip1 in human myeloid leukemia cells induced to differentiate by 1,25-dihydroxyvitamin D3. Cell Cycle 8, 736–741. DOI: 10.4161/cc.8.5.7870