Human Immunodeficiency Virus (HIV) is a retrovirus that attacks the human immune system, leading to acquired immunodeficiency syndrome (AIDS). HIV infects and replicates in CD4+ T lymphocytes, dendritic cells, macrophages, and other immune cells. The pathogenesis of HIV infection involves a complex interplay between the virus, the host immune system, and other factors that influence disease progression.
What is the life cycle of HIV?
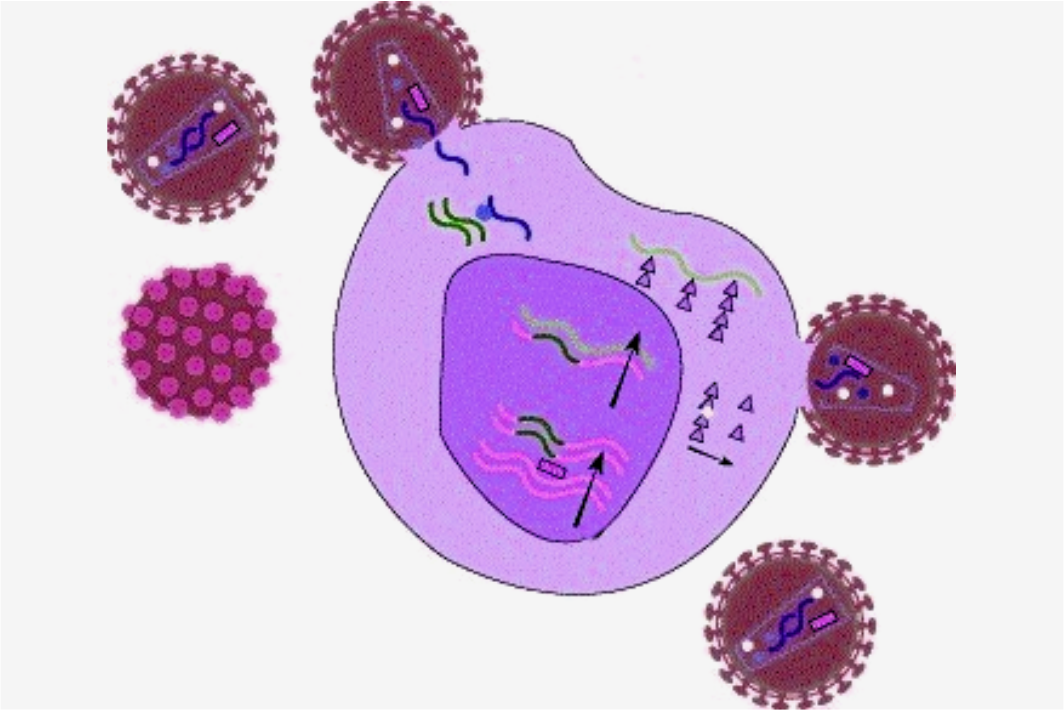
The HIV life cycle begins with the virus bonding to the host cell surface. Next, the viral envelope combines with the host cell membrane, letting go of the viral core into the cytoplasm. The viral RNA genome is then reverse-transcribed into DNA by the viral enzyme reverse transcriptase, which is integrated into the host cell chromosome by the viral integrase enzyme. The integrated provirus can then be transcribed and translated into viral proteins, assembled into new virions, and released from the cell.
How are the immune Responses to HIV?
The host immune response to HIV involves both innate and adaptive immune mechanisms. Innate immune responses include the activation of complement pathways, natural killer (NK) cells, and phagocytic cells such as macrophages and dendritic cells. Adaptive immune responses involve activating CD4+ and CD8+ B cells and T cells and the production of neutralizing antibodies.
CD4+ T cells are critical for generating adaptive immune responses and are the primary target for HIV infection. HIV infection of CD4+ T cells leads to their depletion, resulting in a progressive decline in immune function and the development of AIDS. The virus also induces immune activation and inflammation, contributing to tissue damage and disease progression.
The immune response to HIV is complex and dynamic, with beneficial and harmful effects. HIV-specific CD8+ T cells are associated with controlling viral replication, but their function is often impaired in chronic infection. The production of neutralizing antibodies can prevent viral entry into host cells, but the virus can rapidly mutate to escape antibody recognition. In addition, immune activation and inflammation are thought to contribute to developing non-AIDS-related diseases such as cardiovascular disease, cancer, and neurocognitive impairment.
What factors influence the progression of HIV?
Several factors influence the rate of disease progression in HIV infection. These include the initial viral load and the rate of CD4+ T cell decline, co-infections such as tuberculosis or hepatitis C virus, genetic factors that affect the immune function or viral replication, and environmental factors such as nutrition and stress.
How is HIV managed?
Antiretroviral therapy (ART) has revolutionized the management of HIV infection by suppressing viral replication, preserving immune function, and reducing the risk of transmission. ART consists of combinations of drugs that target different stages of the viral life cycle, including protease inhibitors, reverse transcriptase inhibitors, and integrase inhibitors. ART is typically started when the CD4+ T cell count falls below a certain threshold or when symptoms of AIDS develop.
Conclusion
HIV pathogenesis involves a complex interplay between the virus, the host immune system, and other factors influencing disease progression. Therefore, a better understanding of the mechanisms underlying HIV pathogenesis is essential for developing new therapies and strategies to prevent and treat HIV infection.